SINGAPORE - There is no proven treatment for the coronavirus, so medical care is supportive to give patients their best chance of fighting the disease. Most patients recover on their own, without needing intensive care. The Straits Times speaks to National University Hospital (NUH) doctors at the front lines of the battle against the virus, as they detail the different forms of treatment a patient might go through.
1. Isolation
• Suspected Covid-19 patients are kept in isolation until they are swabbed and tested.
• Lab results are generally available in six to eight hours.
• Once the infection is confirmed, patients are kept in pandemic wards or isolation rooms. Each pandemic ward in NUH holds up to 35 patients.
• In addition to the infectious diseases division, infection control efforts also involve nursing, environmental services, security and engineering.
• For instance, the engineering team helps to design and plan the air flows of the various wards and infection control nurses conduct personal protective equipment training for other departments.
• Only about 5 per cent of patients remain truly asymptomatic, but a larger percentage of individuals may have very mild symptoms which they do not notice.
• Around 40 per cent of transmissions may occur before symptoms manifest.
2. Quarantine and observe
• Around 80 per cent of patients do not need any treatment. They are closely monitored for complications.
• No medication or therapy is used, other than symptomatic treatment such as paracetamol.
• Patients are supported with adequate hydration by making sure they drink water.
What do doctors monitor?
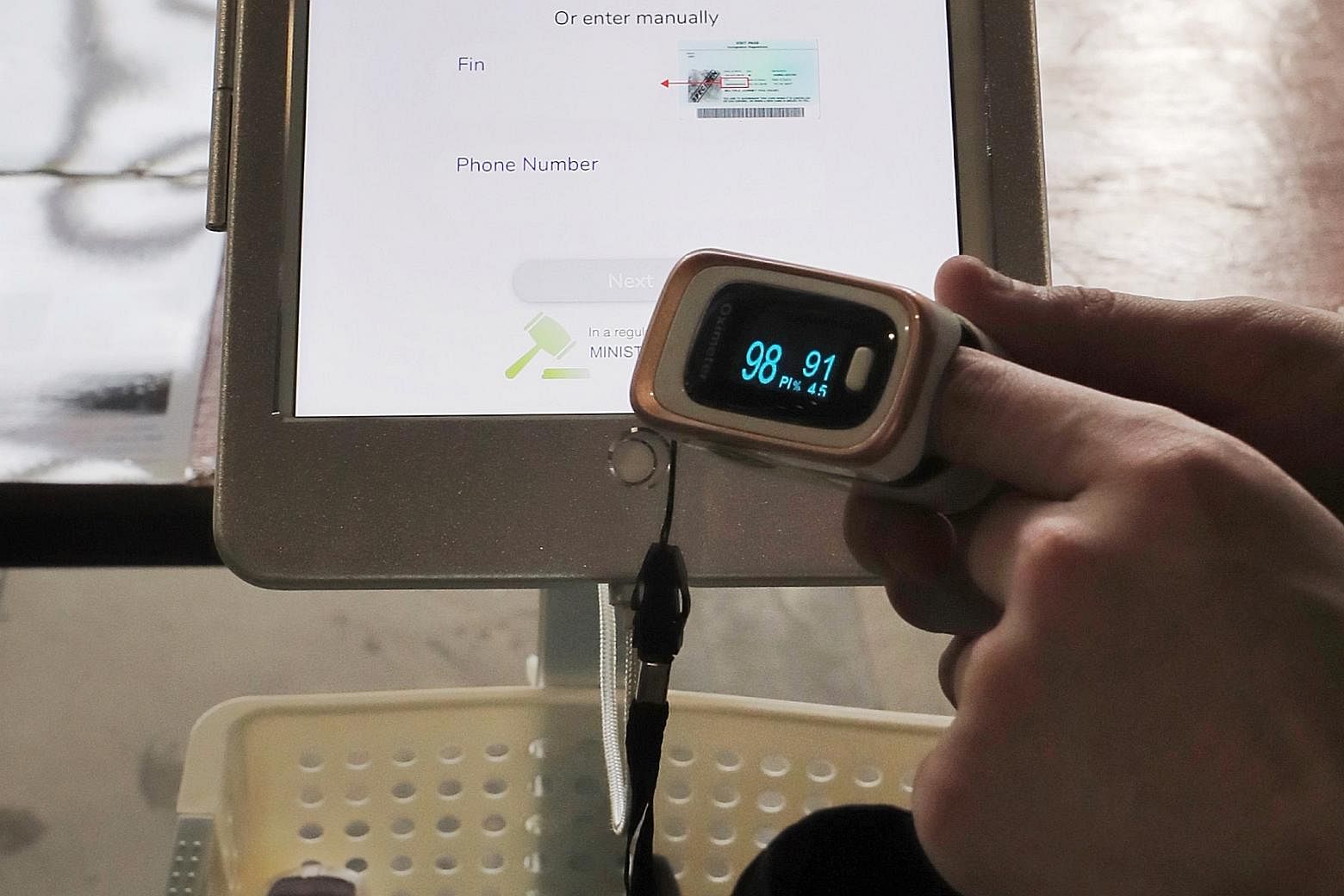
1. Oxygen levels
• Doctors monitor the breathing rate to make sure it is not too high.
• They also look at oxygen levels in the blood using a pulse oximeter: A device which measures oxygen saturation in the blood and heart rate.
2. Chest X-rays
• Doctors look for evidence of pneumonia - which shows up as patches in the lungs.
• This is absent in most children and young adults.
3. Oxygen therapy

• Around 20 per cent of patients need oxygen therapy, though numbers vary from country to country.
• Respiratory rates and blood oxygen levels continue to be monitored.
• Air has only 21 per cent oxygen and the lungs help get the oxygen into the blood.
• When the lungs are damaged, enriched oxygen (up to 50 per cent to 60 per cent oxygen levels) is given by mask or nasal cannulas - tubes inserted into the nostrils.
• Doctors may ask patients to lie on their belly (prone). More blood drains to the front of the lungs via gravity and this improves gas exchange.
4. Non-invasive ventilation

• Fewer than 5 per cent of patients need this.
• Involves the use of machines, such as the bilevel positive airway pressure (Bipap) machine.
• It gives oxygen and pressure to open up airways and is administered by a special mask.
• Bipap machines also generate aerosols that can contain the virus and infect others; hence, healthcare workers must be in full protective gear.
• Some hospitals skip this step completely due to the risks of aerosolising the virus, which will increase the risk of healthcare workers getting infected.
5. Invasive ventilation

• Fewer than 5 per cent of patients need this.
• It is more uncomfortable than non-invasive ventilation.
• Patients have to be sedated and placed in prone position to improve oxygen levels.
• A tube may or may not be placed in the windpipe.
• The tube in the windpipe is more effective as it communicates directly with the lungs and also helps to suck out secretions from the lungs, preventing them from clogging up.
• It is also a closed environment, allowing the virus to remain within the breathing system.
6. Extracorporeal membrane oxygenation (ECMO)

• Fewer than 1 per cent of patients need this.
• It involves a machine that takes over the role of the diseased lung.
• It sucks out blood, which is oxygenated artificially outside the body before being returned into the body.
• Elderly patients are generally too frail to tolerate the effects of ECMO. There will be increased risk of complications, such as bleeding and secondary infections, and these greatly reduce the chances of survival.
• For most patients requiring ECMO, support is given only to the lungs. If heart support is needed, the prognosis is worse.
• Out of all the ECMO Covid-19 patients, fewer than 10 per cent will need ECMO for both the heart and lungs.
NOTE: These are the typical steps which patients might go through, but not all patients will undergo them in the same sequence.
WHEN DO PATIENTS GET ADMITTED TO ICU?
• ICU admission usually happens when non-invasive ventilation is used.
• However, some patients may need ICU treatment earlier if complications develop, such as heart failure, kidney failure, stroke or clot in the lungs.
• In Singapore, patients are generally moved into ICU early when they start to require more than minimal oxygen, so they can be observed.
A POSSIBLE DRUG: REMDESIVIR

• This drug has been shown to speed up recovery times for patients in a major US-led trial.
• At NUH, patients are enrolled in the remdesivir trial when they meet the criteria and give their consent.
WHO ARE THE MEDICAL EXPERTS INVOLVED?
• All stages: infectious disease specialists.
• ICU: infectious disease specialists and ICU specialists in respiratory medicine.
• ECMO: infectious disease specialists, ICU specialists who are experts in ECMO (in NUH and Singapore General Hospital only).
• Cardiologists, haematologists, rheumatologists, renal specialists, psychiatrists and neurologists might also be called in.
• For instance, NUH's first ECMO patient was seen by around 50 specialists at various points in his 42-day hospital stay.
SOURCE: NATIONAL UNIVERSITY HEALTH SYSTEM












